Target general audience: patients with multiple sclerosis and/or anyone generally interested in nutrition and health
Reading time: 6 minutes
Jessica Desamero, PhD
Omega-3s are essential for human health and may even help treat multiple sclerosis, or MS. In a fairly recent study published in the Journal of Biological Chemistry, researchers at the Georgia Institute of Technology and University of Illinois Urbana-Champaign found that compounds derived from omega-3 fatty acids can help control the immune response and reduce MS symptoms in mice1.
What are Fatty Acids and Omega-3s?
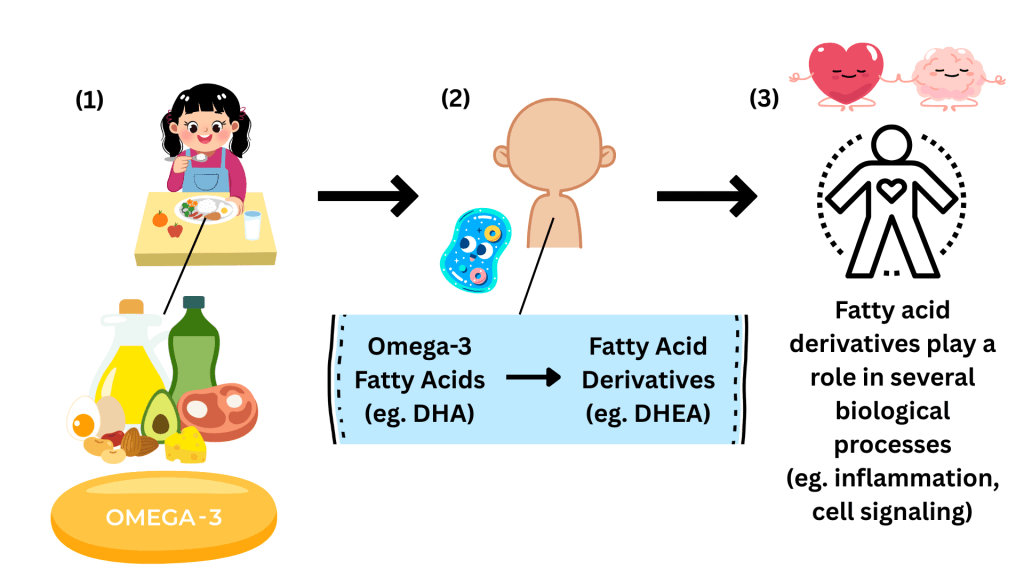
Fatty acids are the building blocks of the fats in our bodies and in the food we eat. Omega-3 fatty acids are a type of healthy, unsaturated fat that can’t be produced sufficiently by the body but can be found in foods like fatty fish, nuts and seeds. Omega-3s are vital because they support several bodily functions, including heart health, eye health and brain function. For example, they can help reduce blood pressure, maintain good vision and improve memory2.
Several omega-3 fatty acids exist, but research studies focus on three main types. One main type is docosahexaenoic acid, or DHA. In addition, once consumed, the body can modify the structures of the fatty acids through chemical reactions. These naturally modified structures are known as fatty acid derivatives, and they play important roles in various biological processes. The fatty acid derivative of DHA is docosahexaenoyl ethanolamide, or DHEA3.
Multiple Sclerosis, Inflammation and Omega-3s: What We Know So Far
Multiple sclerosis, or MS, is a disease in which the immune system mistakenly attacks and eats away at the protective covering of nerves. This nerve damage would cause the brain and body to have trouble communicating4.
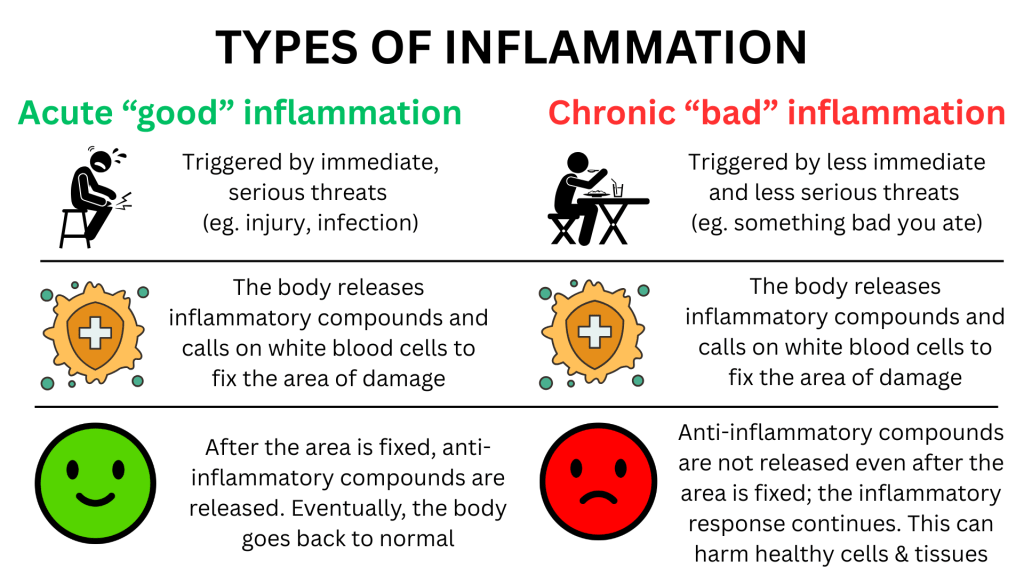
One key feature of MS is chronic inflammation. This is because the immune cells are hyperactive and tend to induce unnecessary proinflammatory responses. Proinflammatory responses involve promoting inflammation at the site of perceived damage. They are a normal way for the immune system to fight infections or injury. However, excessive or prolonged inflammation can be harmful5.
Omega-3s are also known to help reduce inflammation and support immune function. They may even help manage various inflammatory conditions, such as heart disease and autoimmune disorders. Because of this, omega-3s can potentially help manage symptoms of MS as well. Past clinical studies have shown that omega-3-rich diets increased the quality of life for patients with MS. Other previous studies suggest that a DHA-based diet may help slow MS progression. This shows promise for treating this disease with omega-3s and their derivatives. However, it is still unclear how and why this omega-3-MS association happens.
What They Did in Their Research and What They Found
In a past 2017 study, Aditi Das, a professor at Georgia Tech, and her team found that one class of omega-3 fatty acid derivatives reduced inflammation in rat brain tissues and human blood samples. In the recent 2023 study, the team specifically focused on DHEA. In their study, they used mice with a condition that mimics MS called Relapsing-Remitting Experimental Autoimmune Encephalomyelitis, or RR-EAE. In RR-EAE, the immune system attacks the brain and causes brain inflammation6.
Das and her team investigated how DHEA affects the activity of helper T-cells. Helper T-cells are immune cells that play a role in MS progression and RR-EAE induction.
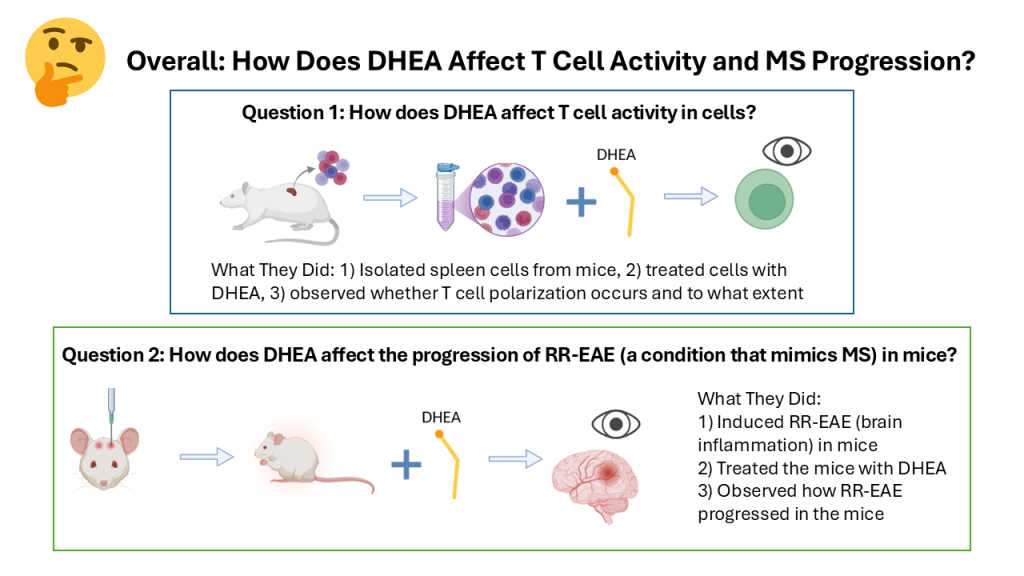
The team first explored how T-cells respond to DHEA in cell culture. They isolated spleen cells from a T-cell-related mouse line, treated these cells with DHEA and then monitored T-cell polarization. T-cell polarization is the process by which the T cells become specialized to fight specific types of threats. In this case, the T cells each become tailored to promote and induce inflammation in their own unique ways. They found that DHEA suppressed T-cell polarization without affecting the proportion of cells that stay alive and functional. This suggests that DHEA can suppress the unneeded proinflammatory immune response. In turn, DHEA may be able to suppress inflammatory diseases.
Later, they explored how DHEA affects the progression of RR-EAE in mice. Here, they induced RR-EAE in mice and treated them with DHEA either at day zero or at the peak of disease. Then they analyzed disease severity based on clinical scores and weight change. “We showed that DHEA can delay the onset as well as the rate of relapse [of RR-EAE] in the multiple sclerosis animal models…That was the most exciting part of the study,” Das said.
The team concluded that DHEA suppresses T-cell responses both in cell culture and in mice and reduces the severity of inflammation in the RR-EAE mice. “A key strength of this research is the use of both cell culture and basic animal models in support of their findings,” said Christopher O’Brien, a neuroscience PhD graduate of Rutgers University-New Brunswick. O’Brien studied stress and opioid abuse susceptibility in mice.
Potential of DHEA in Treating MS
Their study with MS mice models suggests that DHEA may be a promising key agent in managing symptoms more naturally in patients with MS. “The molecule that we’re using is not a targeted drug…It’s a diet-derived molecule that can help,” Das said. “In concert with other medications, this could be very powerful in helping to mitigate symptoms and improve quality of life,” O’Brien said.
Soon, Das plans to test other DHA derivatives and their effects on other types of immune cells, such as B cells. Additionally, some fatty acid derivatives naturally break down and degrade quickly in the body. Therefore, Das wishes to see how to maintain the structure and function of these derivatives to slow their breakdown. This is because by doing so, these derivatives could last longer in cells and help reduce inflammation for a longer time.
Dr. Aditi Das and Dr. Christopher O’Brien were interviewed for this article.
Header Image Source: Greenpeach.com
Figures 1 & 2 were created by the author with Canva.com.
Figure 3 was created by the author, using a combination of Microsoft PowerPoint and BioRender.com.
References
1. Kim JS, Soto-Diaz K, Bingham TW, Steelman AJ, Das A. Role of omega-3 endocannabinoids in the modulation of T-cell activity in a multiple sclerosis experimental autoimmune encephalomyelitis (EAE) model. Journal of Biological Chemistry. 2023;299(2). doi:10.1016/j.jbc.2023.102886
2. Cleveland Clinic. (2022, November 17). Omega-3 Fatty Acids. Cleveland Clinic. https://my.clevelandclinic.org/health/articles/17290-omega-3-fatty-acids
3. Michiel G.J. Balvers, Verhoeckx, K., Pierluigi Plastina, Wortelboer, H. M., Jocelijn Meijerink, & Witkamp, R. F. (2010). Docosahexaenoic acid and eicosapentaenoic acid are converted by 3T3-L1 adipocytes to N-acyl ethanolamines with anti-inflammatory properties. Biochimica et Biophysica Acta – Molecular and Cell Biology of Lipids, 1801(10), 1107–1114. https://doi.org/10.1016/j.bbalip.2010.06.006
4. Goldenberg MM. Multiple Sclerosis Review. P T. 2012;37(3):175-184.
5. Harvard Health Publishing. (2020, April 1). Understanding acute and chronic inflammation. Harvard Health. https://www.health.harvard.edu/staying-healthy/understanding-acute-and-chronic-inflammation
6. Gole S, Anand A. Autoimmune Encephalitis. In: StatPearls. StatPearls Publishing; 2024. Accessed February 29, 2024. http://www.ncbi.nlm.nih.gov/books/NBK578203/

Leave a comment